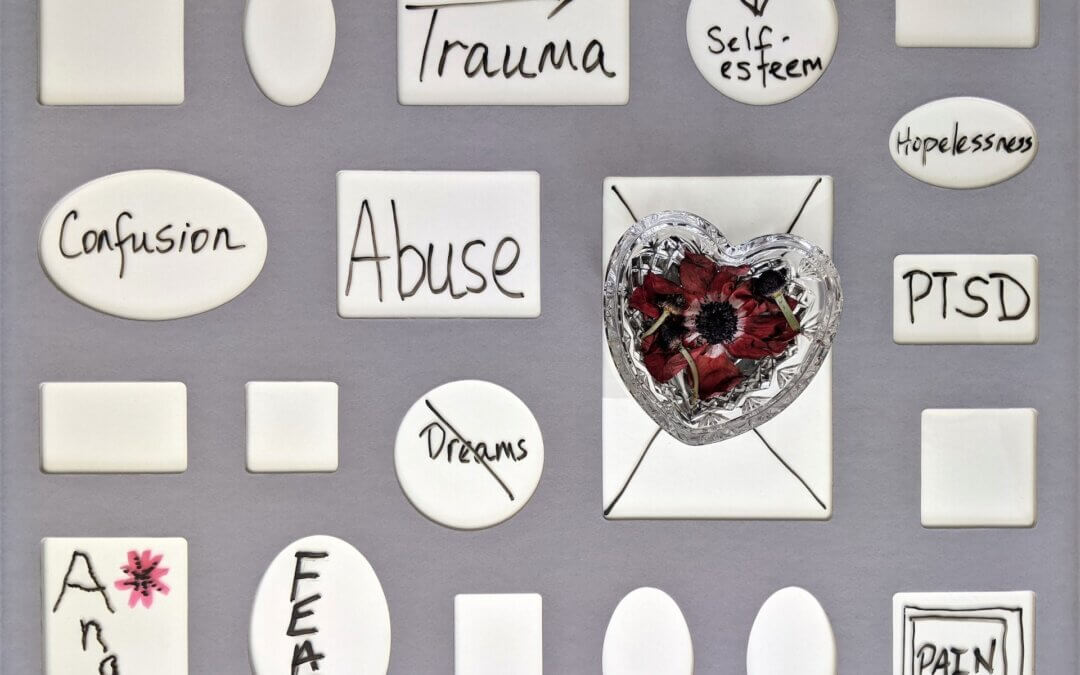
Most people have a basic understanding of PTSD. Unfortunately, that understanding might stem from what you’ve seen in a movie or on a television show. While some of those depictions are more accurate than others, everyone needs to recognize what PTSD really is and what it looks like — especially when it goes undiagnosed.
It’s not easy to think about past trauma. Maybe you’re the one who went through it and you’ve spent years trying to push it down or move forward. But, you could be dealing with undiagnosed PTSD, which makes it more difficult to move on with your life.
What does that look like, exactly? How can you tell if you’re struggling with undiagnosed PTSD? More importantly, what can you do to help yourself, even if you experienced trauma years ago?
Common Symptoms of PTSD
If you’re not sure whether you have PTSD, just look at some of the typical symptoms. They can be slightly different for everyone, but the most common include flashbacks, nightmares, or intrusive memories.
These thoughts and nightmares can seem very vivid and real. They can cause you to experience overwhelming emotions. Or, as a defense mechanism, you might learn to go “numb.”
Undiagnosed PTSD can lead to feelings of emotional numbness that are used to protect your mind from the negative things that happen to you. Unfortunately, it’s a defense mechanism that isn’t built to last. Emotions will always demand to be felt, and even if you push them down or try not to “feel,” it’s likely those emotions will eventually bubble up and be even stronger than before.
What Happens When PTSD Goes Untreated?
The symptoms of PTSD don’t go away even if you try to ignore them. How safe you feel in the world, your ability to trust, to feel alive! In fact, undiagnosed PTSD can lead to more serious mental health conditions, including depression and anxiety. To cope, you might start to rely on substances and risky behaviors.
Undiagnosed PTSD can also make it difficult to maintain healthy relationships. Your mind and your life are completely consumed by what you went through, and it’s hard to hold onto just about anything when you’re stuck in that mindset. In addition to rocky relationships, people with undiagnosed PTSD often also have trouble in their careers. PTSD shadows every area of life. It can prevent you from being the mother, wife, partner, or friend you want to be. You can be so distracted by your trauma that it’s difficult to hold down a job or find success with your work.
PTSD doesn’t get better over time without help. In most cases, it gets work and will start to take over nearly every aspect of your life. Whether you’re purposely trying to “ignore” it or you’re not sure whether you actually have it, getting an official diagnosis is crucial.
How Is PTSD Treated?
A mental health specialist like a psychiatrist or therapist most often diagnoses PTSD. But, it can also be diagnosed by a general physician through a series of tests and conversations. Once you receive a diagnosis, you can work with a therapist who specializes in treating PTSD to find a treatment plan that meets your needs. The US Department of Veterans Affairs (2023) recommends treating PTSD using individual trauma-focused psychotherapy over medications. Based on research, Prolonged Exposure, Cognitive Processing Therapy, and Eye Movement Desensitization and Reprocessing are recommended over medications for PTSD treatment. Each of these effective therapies works a little differently, and it is your preference and fit that matters,
Trauma-Informed Therapy
Trauma-informed therapy recognizes the influence of trauma on individuals. It shifts the narrative from diagnosing and labeling what is wrong to understanding how what happens to you impacts you and how to move toward healing. Trauma-informed therapists have specialist training, skills, and tools that can help people with PTSD. Therapy establishes a space for recovery and fosters resilience.
Next Steps
It’s certainly not easy to “go back” and feel like you have to talk about what happened to you; that’s often the best first step toward true healing. Also, remember that trauma-informed therapy is going to give you the tools and support to address what happened to you. You will not be asked to just talk about your trauma and forced to re-live it. When you start working on your trauma, it will happen in a safe and supportive way. You will have control over what happens in therapy.
Knowing you don’t have to do it alone is empowering and can give you the strength and resolve to start moving forward.
Don’t let the effects of undiagnosed PTSD take over your life. If you’re ready for a diagnosis and an effective treatment plan, reach out to a trauma-informed therapist as soon as possible. You can retake control of your life without having to live with scary, painful memories.
If you want to learn more about the therapy I offer: